Endometriosis: A review on anatomic principles and the management
Dec 20, 2018
Endometriosis should be treated properly in order to preserve the patient’s quality of life and health.
Key Points
Highlights:
- The patients should be informed about complications that might arise from endometriosis.
- The clinicians should be aware of the different atypical presentations and imaging modalities used to diagnose endometriosis.
Objective:
- Authors aimed to examine the known anatomic principles of endometriosis in the literature and outline ways to manage endometriosis patients better.
What's done here:
- Various aspects of endometriosis such as the pathophysiology, the anatomy, the pain mechanism, the perineural spread theory, clinical manifestations, diagnosis, and imaging, infertility, unusual cases, the management, and treatment are explored and assessed in this review paper.
Key Results:
- The most widely accepted theory of the pathophysiology of endometriosis is the implantation, which involves the establishment of an early lesion in the uterus that serves as a nidus for endometrial tissue proliferation.
- The primary symptom of endometriosis patients is pain which consists of two types; visceral (internal organs) and somatic (skin or deep tissues).The pain mechanism in endometriosis is thought to have a nociceptive origin rather than a neuropathic origin, since the pain is disappeared after the surgical removal of the endometriotic lesions, and the central sensitization can be attributed to the inflammatory processes that occur after the non-neural tissue damage in nociceptive pain.
- In deep infiltrating endometriosis patients, the most frequent location of pain was found to be the bowel followed by the uterosacral ligaments; deep dyspareunia was observed to be associated largely with vaginal and rectovaginal septum lesions, with dyschezia related closely to adhesions in the cul-de-sac.
- Endometriosis may spread into the nerves originating from the lumbosacral plexus, including the obturator and sciatic nerves and may also involve the central nervous system. The supporting evidence for this type of spread is that endometriotic lesions’ expression of nerve growth factor and the presence of the nerve growth factor receptor (Trk-A) on the pelvic nerves.
- The gold standard for the diagnosis of endometriosis is laparoscopy with biopsy to demonstrate the histopathological presence of the endometrial tissues. MRI also allows endometriotic lesions and implants to be visualized, which might not be visible via ultrasonography and permits a complete scan of all the pelvic compartments.
- Infertility is a common complication seen in women with moderate to severe endometriosis; it may be caused by endometriotic lesions or implants’ distortion of the normal pelvic anatomy, and interference of increased macrophages and scarring with normal sperm motility and ciliary function as well as the obstruction of the fallopian tubes. The other causative factors are perturbed folliculogenesis secondary to pituitary dysfunction, luteal phase defects, progesterone resistance, and anti-endometrial antibodies.
- Women, less than 35 years of age with endometriosis may have an increased risk of infertility, probably secondary to endometriotic lesions or implants’ distortion of the normal pelvic anatomy.
- Endometriosis should be kept in mind as a probable differential diagnosis in female patients with recurrent pain in extra-pelvic locations lacking a certain etiology.
- Early diagnosis and focused treatment to prevent disease progression and improve patient's quality of life are the aims of management in patients with endometriosis.
- Medical therapy in patients with endometriosis is non-curative and is only used to suppress disease progression. Surgical management is the primary treatment for infertile patients with endometriosis and is also beneficial in patients with severe pain refractory to medical therapy.
- Prolonged use of suppressive medical therapy post-surgery (greater than 6 months) can prevent recurrence of dysmenorrhea in most patients, but has little to no effect in controlling recurrent chronic pelvic pain or dyspareunia.
Lay Summary
In the study of Alimi et al. which has been published in the journal Cureus, various aspects of endometriosis such as the pathophysiology, the anatomy, the pain mechanism, the perineural spread theory, clinical manifestations, diagnosis, and imaging, infertility, unusual cases, the management, and treatment are reviewed.
The hypotheses of the pathophysiology of endometriosis include the implantation or metastatic, metaplasia, induction, and endometriosis disease theories, and most recently, the stem cell theory. Endometriosis that begins with endometrial stem cells tends to be more severe than that which originates from the spread of more differentiated cells, because of the stem cells’ plasticity and the retained ability to attach, differentiate, and proliferate extensively, and therefore exhibit a greater tendency to colonize an ectopic site.
The combination of both visceral and somatic pain that endometriosis patients experience different degrees contributes to the complexity of endometriosis treatment. The pain mechanism that endometriosis patients experience has a nociceptive origin rather than a neuropathic origin. However, endometriosis patients can experience neuropathic pain that is caused by the nerve injury that may occur during the surgery; it may be the cause of recurrent pain in endometriosis patients whose lesions have been removed. Endometriosis may involve nerve tissues in the pelvis as well as the central nervous system. Increased nerve sensitization and pain is seen in endometriosis patients may result from the proliferation of the nerves caused by the expression of nerve growth factor in endometriosis and Trk-A on neural tissues.
Laparoscopy with biopsy is the gold standard for the diagnosis of endometriosis. Pelvic MRI also decreases the likelihood of missing a lesion or implant, and therefore, leads to a better surgical outcome.
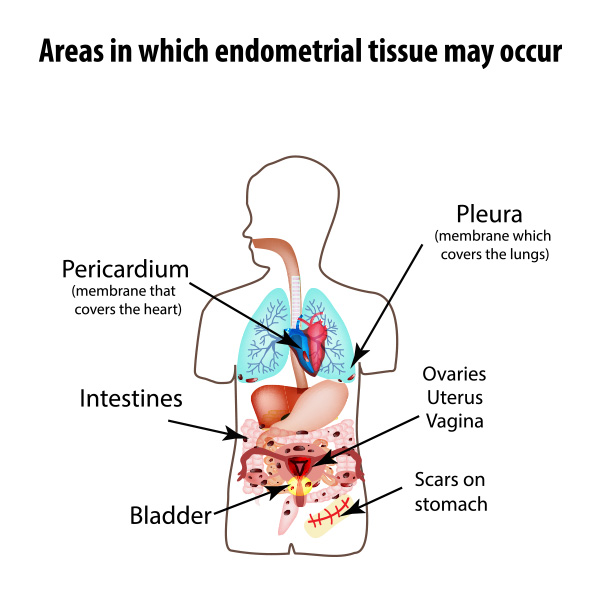
Clinicians should know about the atypical presentations of endometriosis such as the gastrointestinal tract, lungs, liver, pericardium, and brain involvement.
Medical therapy is only used to suppress endometriosis progression, not for the cure of endometriosis or its major complication infertility.
The authors reiterated that the primary treatment for infertile patients with endometriosis is surgery, as it can improve the patient’s probability of spontaneous conception or pave the path for in vitro fertilization. Surgery is the primary treatment for endometriosis patients who are infertile or who have severe pain refractory to medical therapy or who have severe, debilitating, and refractory disease.
Research Source: https://www.ncbi.nlm.nih.gov/pubmed/?term=30510871
endometriosis pelvic pain dysmenorrhea diagnosis management

