Pathophysiology of peritoneal endometriosis pain.
May 20, 2019
Pathophysiology of pain in endometriosis
Key Points
Highlights:
- Through exploring different neuronally active factors in and around ectopic lesions which may be contributing to pain generation, this study provides insight and a better understanding of the pain mechanisms associated with peritoneal endometriosis.
Background:
- Endometriosis may cause different symptoms depending on the location of the lesion, but the severity of anatomic changes caused by endometriosis is not correlated with pain.
- Some patients benefit from hormonal therapy that suppresses menstrual cycles hence the bleeding. Some others do not respond to hormonal therapy and need repetitive surgeries.
What's Done Here:
- This is an invited editorial by Ferrero et al., recently published in Annals of Transitional Medicine. The authors described the pathophysiology and the underlying mechanisms of pain in endometriosis, with reference to the article by Asally et al.
Key Results:
- Endometriotic tissue triggers the formation of new nerve fibers. The menstrual cycles cause bleeding; bleeding triggers inflammation; inflammatory cells and mediators stimulate the nerves which cause pain.
- Nerve fiber density correlates with the intensity of pain in endometriosis.
- Nerve fibers are also more common in superficial endometriosis compared to the normal peritoneum, and more common in deep infiltrating endometriosis than the superficial endometriosis.
- In superficial endometriosis, endometriotic stroma has more nerve fibers.
- In superficial endometriosis, endometriotic glands express molecules related to neuronal guidance (such as persephin, GDNF and NT-4, semaphorin, semaphorin 3E receptor, Skit -2 receptor, Robo-4).
- This nerve development is thought to arise with the help of the factors released from the glandular component.
Lay Summary
This article is an invited editorial by Ferrero S et.al. from IRCCS Ospedale Policlinico San Martino, Genoa, Italy, published in the Annals of Translational Medicine. The authors describe the pathophysiology and underlying mechanisms of pain in peritoneal endometriosis with reference to the article by Asally et al. in Molecular Neurobiology.
Endometriosis may cause different symptoms depending on the location of the lesion. Endometriosis may be a superficial lesion or may infiltrate deeper into the organs.
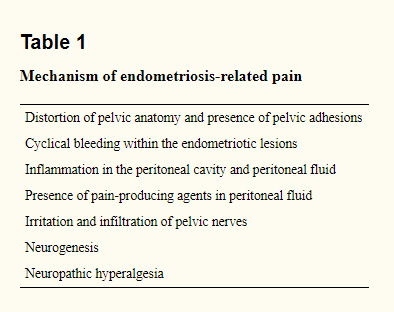 The exact mechanism of pain is still unknown and there are many proposed mechanisms as described in the paper (Table 1).
The exact mechanism of pain is still unknown and there are many proposed mechanisms as described in the paper (Table 1).
Large cysts and deep endometriosis change the anatomic structures with adhesion and bands, however, the severity of anatomic lesion is not correlated with the severity of pain. Endometriotic tissue is hormonally active, which means it responds to hormones and goes into menstruation cycle. The bleeding will yield to inflammation. Inflammatory cells and inflammation mediators sensitize peripheral nerves and cause pain. Nodules may directly irritate or infiltrate the nerves which cause pain.
Endometriotic nodules contain newly formed nerve fibers. Deep infiltrating endometriosis have more nerve fibers than the superficial endometriosis. Also, deep infiltrating endometriosis has more nerves that sense pain. There is a correlation between nerve fiber densities and pain. In addition, superficial peritoneal endometriosis has also been shown that endometriotic stroma has more nerve fibers than adjacent healthy peritoneum.
Glands express molecules related to neuronal guidance. Endometriotic lesions express neurotropic receptors and growth associated proteins (e.g. persephin, GDNF and NT-4, semaphorin, semaphorin 3E receptor, Skit -2 receptor, Robo-4, etc).
The authors suggest that the expression of different neuronally active factors in and around ectopic lesions are the contributors to pain generation. The study improved our understanding of the pain mechanisms associated with peritoneal endometriosis.
Research Source: https://www.ncbi.nlm.nih.gov/pubmed/31032289
endometriosis pain pathophysiology persephin GDNF and NT-4 semaphorin semaphorin 3E receptor Skit -2 receptor Robo-4 Guidance; Neural; Neurotrophin; Peritoneal

