Perineal Endometriosis, How Soon Does it Return After Surgery?
Apr 7, 2021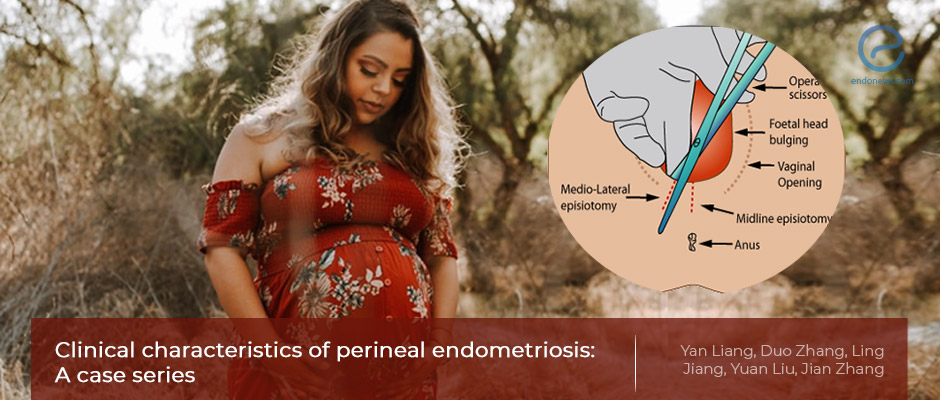
The body mass index (BMI) of a woman at delivery and one month later affects how quickly perineal endometriosis returns after surgery.
Key Points
Highlights:
- Higher BMI at delivery and one month after the delivery shortens the time of symptom return following surgery in women with perineal endometriosis.
Importance:
- The incidence of perineal endometriosis is low, representing only 3 in a thousand women with endometriosis treated by surgery. Both the incidence and clinical characteristics are not well-known.
- Implantation during vaginal delivery is thought to be the etiopathogenetic origin. If so, the incubation period, the time from the last delivery to the time when symptoms appeared, and the factors affecting the disease should be clarified.
- Examining the factors that may be related to the incubation period and pain may help to provide suggestions for the prevention and treatment of the disease.
What's done here:
- Researchers retrospectively analyzed 14 women with perineal endometriosis who underwent resection surgery to treat their disease and gave birth via vaginal delivery.
- All patients had histopathologically confirmed "perineal endometriosis" diagnosis.
- The demographic data, medical history, fertility history, information on the last delivery, symptoms, diagnosis basis, treatment, and outcome were collected, follow-up data including postoperative treatment, pain relief, relapse, and treatment for relapse were recorded.
- All 14 patients had perineal endometriosis secondary to an episiotomy or wound during delivery, and the incubation period ranged from 2-69 months after surgery.
- The factors affecting the occurrence such as age at onset, delivery age, body mass index (BMI) at delivery, BMI within 1 month after delivery, breastfeeding period, the time of return to menses are evaluated.
- The relationship between the incubation period of PEM and other factors was calculated.
Key results:
- Among more than 13500 patients who underwent surgery for endometriosis, 14 had peritoneal endometriosis (1 per 1000 endometriosis patients). During the follow-up for 4-129 months, only one recurred.
- Although the preoperative pain scores were high in perineal lesions, the average pain score at three months following surgery was significantly lower after surgery, compared to before surgery.
- The diameter of the endometriotic lesion in the patient with relapse was 2.5 cm, with the highest pain score before surgery, which dropped after surgery. Recurrence was at the sixth month and no recurrence seen in 28m after her second surgery.
- When the BMI during delivery, and within 1 mo after delivery is high for a patient with endometriosis, the occurrence of perineal endometriosis was earlier.
- Surgical resection is the best treatment option for perineal endometriosis.
- It is very important to evaluate the location of lesions before surgery.
Limitations:
- The sample size in this study was small with only 14 women.
- This was a retrospective study and, therefore, the results may be affected by a recall bias.
Lay Summary
The higher the body mass index (BMI) of a woman during delivery and within one month after delivery, the quicker the symptoms of perineal endometriosis return. This is according to a recent study that appeared in the World Journal of Clinical Cases.
Based on this finding, the authors stress the importance of evaluating the location of endometrial lesions before surgery and recommend immediate surgery following a diagnosis of perineal endometriosis.
Perineal endometriosis is a rare form of endometriosis where hard nodules form in the perineum or the area between the vagina and anus causing pain including period-related pain, pain during intercourse, or pain while passing stools. This has a serious effect on the patients’ quality of life and physical and mental health.
In the present study, a team of researchers led by Dr. Jian Zhang, Chief Doctor in the Department of Obstetrics and Gynecology at the International Peace Maternity and Child Health Hospital in Shanghai, China analyzed factors that may be related to the time it takes for the pain to return after surgery in women with peritoneal endometriosis. Their aim was to suggest ways to prevent and treat peritoneal endometriosis.
The team collected and analyzed clinical and follow-up data from 14 patients with peritoneal endometriosis who visited The International Peace Maternal and Child Health Hospital Affiliated to Shanghai Jiaotong University between January 2009 and December 2019. All patients had had vaginal deliveries and underwent resection surgery to treat their peritoneal endometriosis.
The researchers looked at the BMI of the women at delivery and one month later. They also analyzed the visual analog scale score in the perineal lesions before surgery and three months after surgery. The visual analog scale is a scale that is used to evaluate the severity of pain. They found that BMI at delivery and at one month after delivery was negatively correlated with the time it took for the symptoms to re-appear after surgery. In other words, the higher the women’s BMI was at delivery and one month after, the sooner their symptoms returned after surgery.
The visual analog scale scores of the women were significantly lower compared to before surgery. Only one patient had her disease return within six months after her first surgery and had to have a second surgery. She did not have a relapse until the end of the study.
“Surgical resection of the lesion is the best treatment for [perineal endometriosis] and results in significant alleviation of symptoms," the researchers concluded. They added that immediate surgery is recommended following a diagnosis of perineal endometriosis.
Research Source: https://pubmed.ncbi.nlm.nih.gov/33644167/
BMI Delivery Resection surgery Perineal endometriosis

