Hale Goksever Celik, MD
Hale Goksever Celik, MD
Dr. Goksever Celik is an obstetrician and gynecologist, graduated from the medical school of the Hacettepe University in Ankara, and trained through Obstetrics and Gynecology fellowship at Dokuz Eylul University in Izmir. She has been a postdoctoral research fellow at Molecular Biology and Genetics at Istanbul University. She has been participating in several research especially interested in the association between endometriosis surgery and ovarian reserve and the genetic basis of endometriosis.
Endometriosis Does Not Impair Implantation After Oocyte Donation
Endometriosis is a common gynecological disease that affects up to 40% of women experiencing infertility. It can reduce the chance of pregnancy by damaging the ovaries and lowering the number and quality of eggs, through mechanisms such as chronic inflammation, oxidative stress, and tissue scarring. For women with severe disease, infertility is often one of the most distressing consequences. To better understand whether endometriosis also affects the uterus’s ability to support a pregnancy, researchers from France examined outcomes in women…
Key Points Lay SummaryPsychological Burden of Endometriosis During Assisted Reproduction
For many women, endometriosis is not only a fertility-related diagnosis but a long-term pain condition that can shape daily functioning, intimate life, and emotional well-being. When fertility decisions are on the table, this burden may intensify in distinct ways. In this study published in Fertility and Sterility, Dr. Pietro Santulli and colleagues investigated whether mental health differs between two fertility contexts: women actively trying to conceive through IVF/ICSI and women choosing fertility preservation by freezing oocytes. Participants completed validated screening…
Key Points Lay SummaryEndometriosis and Mental Health: Disentangling Pain and Inflammation
Endometriosis is increasingly recognized as a condition that affects the body far beyond the pelvis, influencing immune function, inflammation, and even emotional wellbeing. Many patients experience symptoms such as chronic pelvic pain, fatigue, and hormonal changes, but the relationship between endometriosis and mental health has remained a subject of debate. Are depression and anxiety primarily a consequence of severe, unrelenting pain, or does the disease itself—through its systemic inflammatory effects—contribute to emotional distress? To explore this question, Goodwin et al.,…
Key Points Lay SummaryEndometrial PreparationMethods and Obstetric Risks After Frozen Embryo Transfer in Endometriosis
Endometriosis is a common condition and is present in 30–50% of women who experience difficulty conceiving. Because it can cause pelvic adhesions, hormonal disturbances, and chronic inflammation, many women with endometriosis require assisted reproductive technologies such as IVF and frozen embryo transfer (FET) to achieve pregnancy. Beyond infertility, endometriosis is also associated with higher risks of obstetric complications, including early pregnancy bleeding, hypertensive disorders, and placental abnormalities. Frozen embryo transfer (FET) is a common part of fertility treatment, and women…
Key Points Lay SummaryFertility and Recurrence Outcomes After Laparoscopic Ethanol Sclerotherapy for Endometriomas
Ethanol sclerotherapy is a minimally invasive approach for treating ovarian endometriomas and is sometimes used as an alternative to surgical cystectomy, particularly when preservation of ovarian reserve is a priority. Instead of removing the cyst wall, the technique involves aspirating the cyst contents and instilling 95–100% ethanol to ablate the lining, with the goal of minimizing damage to healthy ovarian tissue. It is typically considered for larger or recurrent cysts and has a generally favorable safety profile, although recurrence and…
Key Points Lay SummaryEndometriosis Treatments Fall Short in Combating Fatigue
Fatigue is one of the most overlooked but debilitating symptoms in women with endometriosis, often impairing productivity, emotional well-being, and social life. Despite the high prevalence of endometriosis-associated fatigue and significant impact on a person's quality of life, there is limited evidence regarding its management within the current literature. To better understand how current therapies affect this symptom, researchers conducted an international online survey involving nearly 3,000 women with endometriosis. The study, published in Reproduction and Fertility by Kuan et al.…
Key Points Lay SummaryHidden Pain: Increased Self-Harm Risk in Endometriosis
Endometriosis challenges both the body and the mind, revealing how chronic inflammation, pain, and delayed recognition can intersect to shape mental health outcomes. Increasing evidence suggests that the biological mechanisms underlying the disease—particularly immune activation and persistent pain signaling—may heighten psychological vulnerability, even in individuals without prior psychiatric history. In a large population-based study published in Obstetrics & Gynecology, Thiel and colleagues from Ontario, Canada, investigated whether individuals with endometriosis face an increased risk of self-harm and related behaviors. Using…
Key Points Lay SummaryFear of Progression in Endometriosis: The Role of Treatment Approach
Endometriosis is a chronic condition that causes pain, infertility, and a range of mental health challenges, including anxiety and depression. A particular form of anxiety, known as fear of progression, reflects the worry that the disease will worsen over time. This fear can lead to insomnia, fatigue, and disruptions in daily life. A recent study by Dr. Focsa from the Department of Medical Informatics and Biostatistics of Victor Babes University of Medicine and Pharmacy Timisoara, Romania, published in the Journal…
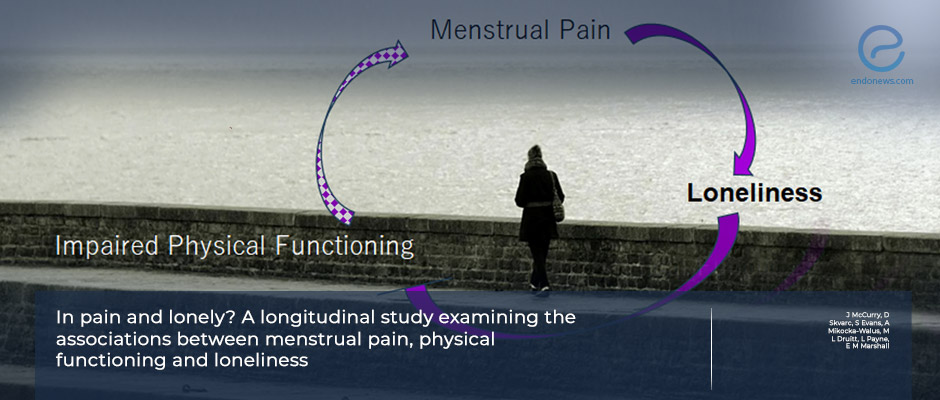
Key Points Lay SummaryMenstrual Pain and Loneliness: The Mediating Role of Physical Functioning
Menstrual pain is one of the most common health problems among menstruating individuals, with moderate-to-severe pain (dysmenorrhea) affecting up to 80%. Beyond its physical and economic burden, the social consequences of menstrual pain are less well understood. In a new longitudinal study published in the British Journal of Health Psychology, McCurry and colleagues investigated whether menstrual pain contributes to loneliness directly, or whether the impact is driven by the way pain impairs daily functioning. The researchers followed nearly 300 Australian…
Key Points Lay SummaryHigh Endometriosis Risk in Obstructive Female Genital Tract Malformations: A 10-Year Surgical Cohort Study
The link between female genital tract congenital anomalies and endometriosis is not fully understood, but these anomalies are known to increase the likelihood of retrograde menstruation—a key mechanism believed to contribute to the disease. In a large retrospective cohort study titled “Endometriosis in patients with female genital tract congenital anomalies: A retrospective cohort study” and published in the Journal of Gynecology Obstetrics and Human Reproduction, Liu et al. from China analyzed data from 675 women with congenital genital tract anomalies…
Key Points Lay SummaryPredictors and Symptom Burden in Adenomyosis-Endometriosis Overlap
Adenomyosis and endometriosis are two gynecological conditions that often overlap but are frequently misunderstood. Adenomyosis occurs when endometrial tissue grows into the muscular wall of the uterus, while endometriosis involves similar tissue growing outside the uterus. Both can cause chronic pelvic pain, heavy menstrual bleeding, and infertility—but when they occur together, symptoms may be more severe and harder to manage. In a recent study published in the Journal of Gynecology Obstetrics and Human Reproduction, researchers from Changsha, China, examined over…
Key Points Lay SummaryCognitive Difficulties in Endometriosis
Endometriosis, a chronic inflammatory condition affecting reproductive-aged women, is increasingly recognized for its impact beyond pelvic pain and infertility. Recent evidence suggests it may also impair cognitive functioning, with symptoms like memory lapses and difficulty concentrating often described as “brain fog.” In a new study published in the Journal of Health Psychology, Dr. Horn and colleagues from Australia surveyed 1,239 individuals with self-reported endometriosis. Using the Functional Assessment of Cancer Therapy-Cognitive Function (FACT-Cog) tool, they found that approximately 80% of…
Key Points Lay SummaryNon-Menstrual Pelvic Symptoms in Endometriosis: Impact on Quality of Life
Endometriosis is a chronic, inflammatory condition where endometrial-like tissue grows outside the uterus. It affects an estimated 6–10% of women of reproductive age and is known for causing painful symptoms such as dysmenorrhea (painful periods), dyspareunia (painful intercourse), chronic pelvic pain, and infertility. A research team led by Fonseca et al. from Brazil recently published a study in PLOS One titled “Non-menstrual pelvic symptoms and women’s quality of life: a cross-sectional observational study.” The study evaluated how non-menstrual pelvic symptoms—especially…
Key Points Lay SummaryClinical Profiles of Adolescents with Histologically Confirmed Endometriosis
Adolescent endometriosis is often underrecognized and underdiagnosed, leading to delayed care and prolonged suffering. In a multi-center study recently published, led by Hewitt al. in the Journal of Pediatric and Adolescent Gynecology, researchers investigated how adolescents with pathology-confirmed endometriosis present clinically and are managed before surgery. The study reviewed the medical records of 305 adolescents under the age of 22 who underwent diagnostic laparoscopy with biopsy-proven endometriosis across eight pediatric academic hospitals in the United States between 2011 and 2021.…
Key Points Lay SummaryRecognizing Adolescent Endometriosis: Early, Intense, and Atypical
Adolescents experiencing pelvic pain often face delayed or missed diagnoses due to atypical symptoms of endometriosis. Unlike in adults, their pain may not follow classic patterns, making it harder to recognize and treat the disease early. In a recent prospective study, the authors led by Dr.Porpora from Italy examined differences in symptom profiles and treatment responses between adolescents (ages 12–18) and adult women with endometriosis. The study, published in the Journal of Clinical Medicine, highlighted striking distinctions in how endometriosis…
Key Points Lay SummaryQuality of Life in Patients with Urinary Tract Endometriosis
Urinary tract endometriosis (UTE) is a specific form of endometriosis that affects the urinary system, most commonly the bladder or urethra. It can cause symptoms such as bladder irritation, urinary urgency, painful urination (dysuria), blood in the urine (hematuria), and loin pain near the kidneys. Pain, a hallmark of endometriosis, often disrupts daily activities, work, and overall quality of life. Beyond physical symptoms, women with UTE may also experience significant emotional distress related to concerns about fertility and surgical outcomes, leading…
Key Points Lay SummaryMultidisciplinary approach in endometriosis patient management
Women with endometriosis suffer from pelvic pain such in terms of dysmenorrhea, dyspareunia or infertility, all of which significantly negatively impact quality of life, and increase the risk of mental health disorders. Hartnett et al., a research team from Ireland, have published a systematic review protocol titled “Cross-disciplinary working between gynaecologists and mental healthcare professionals: a mixed-methods systematic review” in the BMJ Open. The review aims to explore the clinical need for integrated mental healthcare in the context of gynecological conditions…
Key Points Lay SummaryThe Role of Surgeon Specialty in Colorectal Resection Outcomes for Women with Endometriosis
When endometriosis invade the tissues, including the bowel wall by more than 5 mm, it is termed deep infiltrating endometriosis. Patients with bowel involvement typically experience symptoms such as constipation, diarrhea, tenesmus, and rectal bleeding. Surgical intervention is often the primary treatment option for these patients, offering significant improvements in pain, infertility, and digestive issues. Both gynecologists and general/colorectal surgeons are capable of performing this procedure. A study by Nasseri et al., published in Colorectal Disease, sought to explore whether…
Key Points Lay SummaryExploring the Impact of NNMT Enzyme on Endometriosis
Endometriosis is driven largely by inflammation and immune dysfunction. Despite extensive research, the optimal treatment for endometriosis remains uncertain. A better understanding of the disease's mechanisms could lead to improved therapies and a better quality of life for affected women. A recent study by Hou et al., titled "Overexpressed Nicotinamide N‑methyltransferase in Endometrial Stromal Cells Induced by Macrophages and Estradiol Contributes to Cell Proliferation in Endometriosis", published in Cell Death Discovery, investigated the role of nicotinamide N‑methyltransferase (NNMT) in endometriosis.…
Key Points Lay SummaryMay it be a new non-hormonal treatment option for endometriosis patients?
Heidi Ledford published a news in Nature, entitled “How understudied endometriosis causes pain for hundreds of millions of women”. She aimed to summarize the recent status about endometriosis treatment options. Pain-sensing nerves and immune cells interact to worsen both pain and lesion growth in endometriosis. In a study published in Science Translational Medicine, researchers found that the protein CGRP, which mediates communication between these cells, contributes to both the sensation of pain and the progression of lesions in a mouse…
Key Points Lay Summary